Three-dimensional printing (3DP), also known as additive manufacturing, rapid prototyping technology, free-forming technology, etc., is based on the principle of discrete-stacking, using computer-assisted layering and superposition molding techniques. Material is added layer by layer to form a 3D solid. Since the concept of 3D printing technology was first proposed by Charles W. Hull in 1986, 3D printing has penetrated into all walks of life and led innovation, resulting in global manufacturing due to its unique advantages in high precision, personalized manufacturing and complex shape construction. Industry change. Biological 3D printing is a cross-application of 3D printing technology in the field of biomedicine, which has important research significance and application prospects. 3D printing technology can be used to create standard models, as well as tailor-made surgical stents for patients. The patient’s bone defect is scanned by medical imaging techniques such as computed tomography (CT) or nuclear magnetic resonance (MRI) to obtain the desired stent model, which is then printed using a three-dimensional printer. This is difficult to achieve with traditional molding techniques. In recent years, 3D printing technology has been widely used in the medical field, including craniofacial transplantation, crown restoration, prosthetic devices, medical equipment, surgical models, organ printing, drug delivery models, bone tissue engineering stents, etc. [1]. 3D printing technology has attracted wide attention from researchers due to its tailorability, structural and pore controllability, and the ability to composite multiple materials. This trend has also inspired many inventions with breakthrough treatments and devices.
Next we will detail the biomaterials currently available for 3D printing in the field of bone tissue engineering, including their respective strengths and weaknesses and printing standards. At the same time, because different printers can print different biomaterials, we also give a brief overview of the types and molding principles of 3D printers. We hope that this review will encourage more research teams to invent new biomaterials, and ultimately make 3D printing technology more developed in the field of bone tissue engineering.
1. Introduction to 3D printing technology classification
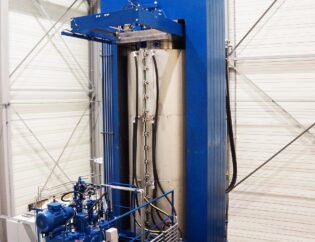
Whether or not biomaterials can be printed has a lot to do with the 3D printers used. Different printers have different material requirements. In the field of biomedicine, the main printers used are divided into four types: photocuring stereo printing technology, fused deposition printing technology, selective laser sintering technology, and direct slurry extrusion technology.
Fused deposition and direct slurry extrusion techniques are two commonly used methods for preparing bone tissue engineering scaffolds. Some directly printed pastes are polymer solutions that are mixed with water or low boiling solvents (dichloromethane (DCM), dimethyl sulfoxide (DMSO), some are polymer solutions that evaporate quickly after extrusion, or Some hydrogels retain their original structure after extrusion. Hydrogels that are formed by three-dimensional printing can be maintained in shape by thixotropic behavior, temperature sensing, or cross-linking after extrusion. For fused deposition and direct printing. The resolution can be as high as 25 microns in the XY plane, and the layer thickness is 200-500 microns [2]. In general, these two methods have problems when printing long unsupported or sharp-pointed models. The filaments do not have enough strength to support themselves immediately, so there is a slack or complete collapse in the unsupported part. To solve this problem, sometimes the filling material is added during the printing process, after the printing is completed. It is dissolved in a solvent or calcined at a high temperature.
Particle-melting 3D printing technology has been widely used in industrial prototyping, including selective laser sintering deposition technology and particle adhesion technology, which not only prints polymers, ceramics, metals and their composites, but also gives them unique Or a complicated structure. Selective laser sintering uses a laser with a specific orientation to bring the polymer or metal particles above their melting point, thereby melting the particles together. The laser beam is layered according to the computer model, and the particles are melted from the top, and this step is repeated to achieve the final result [3]. Selective laser technology is slower to build, more costly, and requires the use of a large amount of material, but its ability to form multiple materials on a single machine tool still makes it a hit in many manufacturing areas. Particle bonding technology is also known as non-directional laser sintering technology, and its main principle is similar to selective laser sintering technology. However, unlike laser melting of particles, the particle bonding technique uses a liquid binder solution to bond the particles and then obtain a three-dimensional solid by high temperature calcination. Selective laser sintering techniques and particle adhesion techniques have been used in hard tissue engineering such as orthopedics or oral surgery.
Stereolithography is the process of forming ultraviolet light or laser light through a photopolymerizable liquid polymer to form a single, rigid polymer film. After polymerization, the substrate is lowered into the solution so that a new resin can flow over the printed surface and polymerize above. Among all printing technologies, stereo lithography has the highest resolution, the traditional stereo lithography resolution reaches 25 microns, while micro-scale stereo lithography and high-precision stereo lithography have a resolution of single micron [4] ]. However, due to stereolithography, it can only be cross-linked under ultraviolet light, extended post-forming properties, lack of proper mechanical properties, resin is easily blocked at the end, and most importantly lacks relevant biological phases that can be used for stereolithography. Capacitive and biodegradable materials make it lack of room for development in the medical field. However, in recent years, the discovery of some natural or synthetic crosslinkable biomaterials has provided great opportunities for the application of stereolithography in the field of tissue engineering [5].
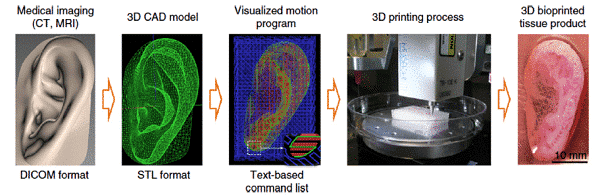
Figure 1 How to print an ear [6]
2. Three-dimensional printing biomedical material classification
In the past ten years, 3D printing technology has been rapidly developed, which has also enabled it to be applied in many new fields, and it has attracted the attention of medical equipment and tissue engineering. Because 3D printing can tailor specific medical products to patients in a short time and low cost, this also makes 3D printing technology have great development prospects in the future personal medical era. At present, there are many biological materials to prepare bone tissue engineering scaffolds or other medical products by means of three-dimensional printing. In this session, we will provide an overview of the material properties required for different printing technologies,and highlight the biomaterials that have been applied and their advantages and disadvantages.
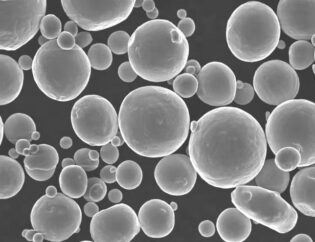
2.1 Ceramic base slurry
Biomedical active ceramics are ideal for bionic bone repair materials by simulating the mineral phase, structure and mechanical properties of natural bone. It is currently difficult to directly print ceramic materials using 3D printers because liquid ceramic materials are small in number and their melting point is far beyond the range that fused deposition printing can withstand. In addition, ceramic materials are not suitable for photocuring three-dimensional printing technology because of their lack of photosensitive properties. It is also difficult to print a high density and porous structure using a selective laser sintering printing system. Direct extrusion 3D printing technology is currently the most promising method for printing ceramic materials. Ceramic powder must have a suitable particle size (usually 10-150 microns) and a suitable bonding solution to make it easy to print. Molding [7].
Hydroxyapatite powder is widely used in three-dimensional printing, which is related to the large amount of calcium phosphate in its mineral phase. The polyacrylic solution was sputtered onto the HA powder layer by layer, followed by sintering to complete the curing process, so that we obtained a hydroxyapatite coupling. Through sintering, its compressive strength (0.5-12Mpa) can meet the minimum requirements of human cancellous bone. It was transplanted into a mouse model, and after 8 weeks, new bone formation began at the edge of the stent, and osteoids and blood vessels grew inside. However, despite the excellent performance of the artificial bone scaffold, it is still far from the clinical use standard [8]. Bioglass is an aggregate of silicates in which internal molecules are randomly arranged. The components in the material can exchange or react with components in the living body to form a substance compatible with the organism itself. The researchers conducted a series of studies on bioactive glass through cell and animal experiments, and found that bioglass has superior self-degradability, and its ion product can enhance the proliferation and differentiation of osteoblasts and activate the expression of osteogenic genes. In order to effectively treat tumor-related bone defect disorders, Lu et al [9] first prepared magnetic nanoparticle-modified mesoporous bioglass and mixed it with chitosan to prepare a porous composite scaffold. The composite scaffold has good bone regeneration and photothermal therapy functions, and has great application value in the treatment of tumor-related bone defects.
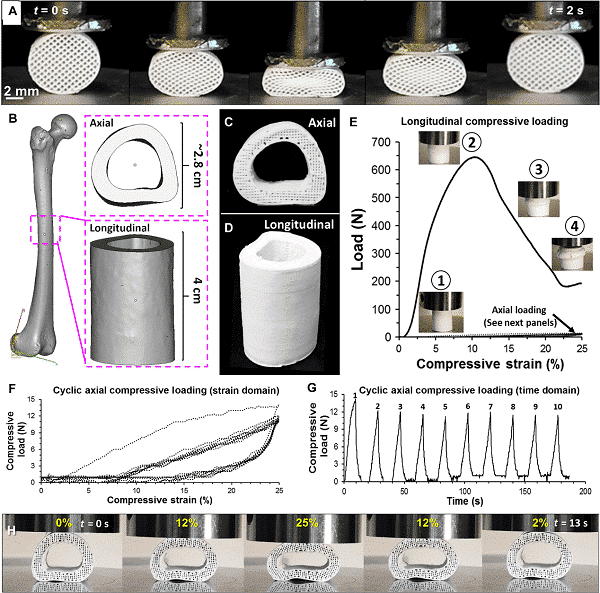
Figure 2 Superelastic artificial bone [10]
2.1 Biomedical polymer materials
Medical polymer printing materials have excellent processing properties, can be applied to a variety of printing modes, and have good biocompatibility and degradability, making them the main force in 3D printing biomaterials. Different printing techniques require different material printing parameters to be set. For example, the fused deposition printing uses a thermoplastic polymer material, which can be printed by simply pulling the raw material into a filament shape, but its diameter is usually about 1.75 mm, and it has a fast solid solution conversion property to ensure that it is squeezed. It melts quickly before going out and can be cooled quickly after extrusion. Photocuring three-dimensional printing technology requires that the slurry be in a liquid state and have photosensitive properties.
At present, the most widely used three-dimensional printing polymer materials are degradable aliphatic polyester materials, such as polylactic acid (PLA) and polycaprolactone (PCL). Polycaprolactone is a semi-crystalline polymer that was once abandoned until the rise of tissue engineering and 3D printing, and PCL is once again on the historical stage. Polycaprolactone has excellent rheological properties and viscoelastic properties when heated, making it one of the most important materials for printers based on fused deposition. Polycaprolactone is stable in the body for up to six months, followed by gradual degradation, and by-products are non-toxic and harmless to the human body. Polylactic acid is a linear thermoplastic aliphatic polyester with good biocompatibility and biodegradability. However, since the degradation of polylactic acid is achieved by hydrolysis of ester bonds, the release of lactic acid causes a decrease in the pH value in the surrounding body fluid environment. These acidic by-products are prone to tissue inflammation and cell death. To improve this problem, the researchers combined polylactic acid with bioceramics to prepare composite scaffolds to improve their bioresponsiveness and impede the formation of acidic environments. Ion et al [11] used a 3D printing technique to fabricate a novel apatite-wollastonite/polylactic acid (AW/PLA) composite structure that matches the properties of cortical and cancellous bone. The results of in vitro cell experiments showed that AW/PLA composite scaffold can effectively promote the proliferation and osteogenic differentiation of rat bone marrow-derived mesenchymal stem cells. In the rat skull defect model, the composite scaffold showed good osseointegration and the ability to promote new bone formation.
In addition to PLA and PCL, polypropylene (PPF) is one of the most studied biodegradable and photocrosslinkable polymer materials in photocuring. Usually, the printed paste is mixed with diethyl fumarate DEF solvent, and a photoinitiator is also added. The viscosity of the solution and the ratio of PPF to DEF have a large effect on the printing process and the mechanical properties of the stent. Polyetheretherketone (PEEK) can only be formed by selective laser sintering printing technology because of its melting point of 350 °C. However, the high melting point also gives PEEK heat resistance, which makes it stable during high temperature steam sterilization. However, as a biological material, PPEK lacks osseointegration favorable for tissue engineering and cannot be well combined with natural bone, so it is easy to cause some rejection reactions, and the price is expensive [12].
2.3 hydrogel slurry
A hydrogel is a polymer formed by chemical crosslinking or physical crosslinking of a water-soluble polymer, has a three-dimensional crosslinked network structure, and also contains a large amount of water itself. The hydrogel has the properties of adjustable strength, degradability, functional modification, etc., and can be used as a soft material to mimic the microenvironment of the extracellular matrix, which makes the hydrogel have broad application prospects in the medical field. It can be used to prepare two- or three-dimensional tissue engineering scaffolds and controlled release of drugs. Commonly used three-dimensionally printed hydrogel pastes are mainly divided into three categories: one is prepared from natural polymers, such as alginate, agar, gelatin, cellulose, collagen, silk fibroin, hyaluronic acid, etc. One type is prepared from synthetic polymers such as polyacrylamide, polyurethane, polyethylene glycol, etc.; the other is a composite hydrogel-based slurry composed of a synthetic polymer and a natural polymer.
Among the water-soluble synthetic polymers, medical polyvinyl alcohol (PVA) is widely used in the field of tissue engineering. PVA has good biocompatibility, is non-toxic and easily degradable, can be dissolved in water at 95 ° C, forms a gel, and has a high viscosity. Zhang et al [13] prepared MBG/PVA composite scaffolds with interconnected pores. The addition of PVA significantly enhanced the toughness of the materials. Animal experiments using a rat skull bone defect model also showed that the MBG/PVA scaffold has excellent osteoinductive activity and promotes new bone formation and angiogenesis at the bone defect.
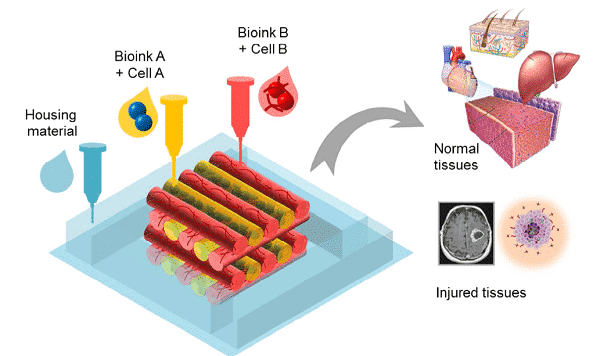
At present, there have been many experiments in which cells are co-cultured with 3D-printed bioscaffolds. The results also show that cells can survive on a variety of three-dimensional scaffolds and are better than ordinary two-dimensional cultures. But this is only a two-dimensional effect of cells and materials, and does not place cells directly in the printing system. The direct mixing of cells with the paste for printing as a new idea has also attracted widespread attention from researchers. Natural hydrogels have good cytocompatibility. Its composition is similar to that of the extracellular matrix, and its ability to adhere to proteins and cells on the surface is weak, and it hardly affects the metabolic process of cells. It can wrap cells, transport nutrients and secrete metabolites. Andrea et al. [14] tested bio-ink formulations of type I collagen and hyaluronic acid in different proportions, and determined an optimal formulation that allows bioprinting while supporting biological activity and supports native cell-matrix interactions. . They applied the formulation to the construction of 3D liver tissue containing human primary hepatocytes and hepatic stellate cells and tested the effects of acetaminophen, a common liver toxicant. The results show that the combination of methyl methacrylate collagen and thiol hyaluronic acid produces a simple, printable bio-ink that regulates the growth of mesenchymal cells and treats drugs. Have the right reaction.
Figure 3 Cell Bioprinting
3. Conclusions and prospects
Three-dimensional printing technology has great application prospects, but there are still many problems to be solved as the main members of the biomedical field. One of the problems lies in the limitations of the 3D printer’s own capabilities. Although its printing speed and printing accuracy have been greatly improved, in many cases it still cannot achieve the best level. Another major problem is the limitations of alternative biomaterials. Although many materials that can be printed have their own advantages, the materials used for transplantation must meet the requirements of physiological conditions and have a good response to the human body. In general, ideal orthopedic materials require the following characteristics: (1) printability, (2) biocompatibility, (3) excellent mechanical properties, (4) good degradability, and (5) by-products. Non-toxic and degradable, (6) good tissue biomimetic properties. Different types of printers have different material requirements, and these characteristics are sometimes difficult to fully satisfy. For example, in bone tissue engineering, on the one hand, a high-strength scaffold material is required to meet the growth and load of osteoblasts, but this also causes a problem of difficulty in scaffold degradation. Some soft materials with low strength are easy to print and are easily degraded, but they cannot be applied to load-bearing parts. In general, three-dimensionally printed pastes are used in the field of bone and cartilage repair due to their own hardness and natural bone proximity. Fundamentally, the choice of biomaterials is to balance their performance to achieve the desired material.
Polymer bio-slurry has been extensively studied, especially for inexpensive elastomers such as PLA and PCL. These materials have excellent biocompatibility and mechanical properties and are widely used as substrate materials. In addition to these, in the future research, attention should be paid to the degradability, brittleness and cytocompatibility of polymer materials. Ceramic materials, such as HA and β-TCP, have traditionally been considered ideal materials for hard tissue engineering scaffolds, and are now increasingly being used in the study of ceramic and polymer composites. The addition of ceramic materials can be improved. The strength of the stent and the biological properties of the composite. The development of hydrogel bio-slurry and the printing system have brought us closer to the printing of multi-functional, cell-mounted model systems, and we have hoped that organ printing will one day be realized. This process has begun with the study of supramolecular hydrogel slurry. Finally, if 3D printing technology is to be applied to the medical field, how to carry out mass production, how to control quality, and how to overcome management obstacles are all problems that need to be solved. Although the front road is long and long, 3D printing will eventually shine in the field of tissue engineering and medicine!
Reference
[1] Murphy S V, Atala A. 3D bioprinting of tissues and organs[J]. Nature Biotechnology, 2014, 32(8): 773-785.
[2] Guvendiren M, Molde J, Soares R M D, et al. Designing Biomaterials for 3D Printing[J]. ACS Biomaterials Science & Engineering, 2016.
[3] Vermeulen M, Claessens T, Van Der Smissen, Van Holsbeke, De Backer, Van Ransbeeck, Verdonck. Manufacturing of patient-specific optically accessible airway models by fused deposition modeling. Rapid Prototyping Journal 2013, 19 (5), 312?318.
[4] Bertrand P, Bayle F, Combe C, Goeuriot P, Smurov I. Ceramic components manufacturing by selective laser sintering. Appl. Surf. Sci. 2007, 254 (4), 989?992.
[5] Derby B. Printing and prototyping of tissues and scaffolds[J]. Science, 2012, 338(6109): 921-6.
[6] Kang, H.-W.; Lee, S. J.; Ko, I. K.; Kengla, C.; Yoo, J. J.; Atala, A. A 3D bioprinting system to produce human-scale tissue constructs with structural integrity. Nat. Biotechnol. 2016, 34 (3), 312?319.
[7] Xiaoyu Du, Shengyang Fu, Yufang Zhu. 3D printing of ceramic-based sca?olds for bone tissue engineering: an overview. Journal of materials chemistry B, 2018,6:4397-4412.
[8] Fierz F C, Beckmann F, Huser M, etc. The morphology of anisotropic 3D-printed hydroxyapatite scaffolds. Biomaterials, 2008, 29 (28), 3799?3806.
[9] Jiawei Lu, Fan Yang, Qinfei Ke, Xuetao Xie, Yaping Guo. Magnetic nanoparticles modified-porous scaffolds for bone regeneration and photothermal therapy against tumors. Nanomedicine, 2018, 14(3):811-822
[10] A.E. Jakus, A.L. Rutz, S.W. Jordan, A. Kannan, S.M. Mitchell, C. Yun, K.D. Koube, S.C. Yoo, H.E. Whiteley, C.P. Richter, R.D. Galiano, W.K. Hsu, S.R. Stock, E.L. Hsu, R.N. Shah, Hyperelastic “bone”: A highly versatile, growth factor-free, osteoregenerative, scalable, and surgically friendly biomaterial, Sci Transl Med, 2016, 8:358.
[11] Ion Tcacencu, Natacha Rodrigues, Naif Alharbi, Matthew Benning, etc. Osseointegration of porous apatite-wollastonite and poly(lactic acid) composite structures created using 3D printing techniques. Mater Sci Eng C Mater Biol Appl, 2018, 90:1-7.
[12] Hoath S. D, Vadillo D. C, Harlen O. G, McIlroy C, Morrison N. F, Hsiao W. K, Tuladhar T. R, Jung S, Martin G. D, Hutchings I. M. Inkjet printing of weakly elastic polymer solutions. J. Non-Newtonian Fluid Mech. 2014, 205,1?10.
[13] Zhang, J. H.; Zhao, S. C.; Zhu, Y. F.; Huang, Y. J.; Zhu, M.; Tao, C. L.; Zhang, C. Q. Three-dimensional printing of strontiumcontaining mesoporous bioactive glass scaffolds for bone regeneration. Acta Biomater. 2014, 10 (5), 2269?2281.
[14] Andrea Mazzocchi, Mahesh Devarasetty, Richard Huntwork, Shay Soker, Aleksander Skardal. Optimization of collagen type I-hyaluronan hybrid bioink for 3D bioprinted liver microenvironments. Biofabrication, 2018, 11(1):015003.